JOURNAL OF THE DENTAL ASSOCIATION OF THAILAND
1
Page : 252-261Title : Fracture Resistance of Endodontically Treated Upper Premolar with MOD Cavity Restored by Direct Resin Composite Combined with Fiber-Reinforced Composite Posts
Author(s) : Chaiwat Maneenut, Nadaprapai Khwanpuang
Keyword(s) : Endodontically treated premolar,Fiber-reinforced composite post,Fracture strength,Resin composite
Manuscript Type : Original Article (บทวิทยาการ)
Page : 252-261
2
Page : 262-273Title : Comparative the Bacterial Aerosol Contamination during Ultrasonic Scaling of Two Type of Ultrasonic Scalers
Author(s) : Suchaya Jirapintu, Romanee Kudngaongarm, Suwunna Tienungoon
Keyword(s) : ฺBacterial aerosol,Ultrasonic scaling,Ultrasonic scalers,Magnetostrictive scaler,Piezoelectric scaler
Manuscript Type : Original Article (บทวิทยาการ)
Page : 262-273
piezoelectric scaler at all sites (p= 0.012, 0.036, and 0.036). In addition, the number of bacterial counts was the highest at the patient’s chest areas (99.50 CFUs). The average bacterial counts from using both types of ultrasonic scalers were significantly reduced at 30 and 60 minutes after ultrasonic scaling (p<0.05). This study indicates that the magnetostrictive ultrasonic scaler produces the bacterial aerosol contamination greater than the piezoelectric ultrasonic scaler. Moreover, both types of these ultrasonic scalers are dramatically decreased at 30 minutes after ultrasonic scaling (p<0.05).
3
Page : 274-279Title : Interobserver Agreement in Proximal Caries Detection from a Smartphone Display
Author(s) : Napas Lappanakokiat, Soontra Panmekiate
Keyword(s) : Bacterial aerosol,Ultrasonic scaling,Ultrasonic Scalers,Magnetostrictive scaler,Piezoelectric scaler
Manuscript Type : Original Article (บทวิทยาการ)
Page : 274-279
4
Page : 280-289Title : In-vitro Remineralization of Dentine Carious Lesions after Application of Silver Diamine Fluoride (Thai Product) Compared with Commercial Brand
Author(s) : Chutima Trairatvorakul, Kantaporn Kunpanichakit, Oranuch Techatharatip, Tirayut Vilaivan, Panida Thanyasrisung
Keyword(s) : Remineralization,Lesion Depth,Mineral Density,Silver Diamine Fluoride,Dentine Carious Lesion
Manuscript Type : Original Article (บทวิทยาการ)
Page : 280-289
determined using a micro-computed tomography (micro-CT) that was used to calculated lesion depth (LD) and mean mineral density (mean MD). The samples were randomized into three groups: SDF (Thai product), commercial SDF (Saforide®: Toyo Seiyaku Kesei, Japan) and deionized water (control group), respectively. After undergoing a bacterial pH-cycling challenge, the samples were re-evaluated for MD and the LD, mean MD, %LD change and %MD change was calculated. The results demonstrated that the mean %MD change of the three groups were 38.9 ± 18.1, 60.2 ± 30.6 and 4.5 ± 7.6 respectively. The mean %MD change in the SDF (Thai product) and Saforide® groups were comparable but significantly different higher that the control (p<0.001). The LD at baseline and post-test of each group did not significantly change (p>0.05). In conclusion, SDF (Thai product) and Saforide® have a similar efficacy in remineralizing dentine carious lesions in primary teeth
5
Page : 290-296Title : Effect of Vitamin C Suspension on Micro Tensile Bond Strength of Non-vital Bleached Dentin to Resin Composite Restoration
Author(s) : Boondarick Niyatiwatchanchai, Chaiwat Maneenut
Keyword(s) : Antioxidant,Bleaching,Bond strength,Micro tensile,Vitamin C
Manuscript Type : Original Article (บทวิทยาการ)
Page : 290-296
6
Page : 297-304Title : Influence of Curved Root Canal on Retreatment Efficacy of Bioceramic Sealer
Author(s) : Piyanee Panitvisai, Kasemsun Sujaritwanit
Keyword(s) : Retreatment,Curved root canal,MicroCT,Bioceramic sealer
Manuscript Type : Original Article (บทวิทยาการ)
Page : 297-304
7
Page : 305-311Title : Dispersion of Microorganisms in the Air During Oral Surgical Procedure Using Low Speed Micromotor
Author(s) : Keskanya Subbalekha, Siriphun Kattapong, Ruchanee Ampornaramveth
Keyword(s) : Dispersion,Micromotor,Bacteria in the air,Fungus in the air,Oral surgery
Manuscript Type : Original Article (บทวิทยาการ)
Page : 305-311
8
Page : 312-319Title : The Mental Index and Panoramic Mandibular Index in Elderly Patients: A Preliminary Cross-Sectional Study
Author(s) : Sorasun Rungsiyanont, Sineepat Talungchit, Sukritta Sirijindanameerat, Paktheema Phoontongphan, Viya Songsomboon
Keyword(s) : Bone mineral density,Mental Index,Panoramic Mandibular Index,Panoramic film,Osteoporosis
Manuscript Type : Original Article (บทวิทยาการ)
Page : 312-319
1
Page : 170-181Title : The Usage of Nasoform in Two Newborns with Unilateral Cleft Lip: Case Reports
Author(s) : Panarat Kodkeaw, Ubonwan Sermchaiwong, Krit Khwanngern
Keyword(s) : Nasoform,Nasoalveolar molding,NAM,Cleft lip,Cleft lip and cleft palate,Nasal molding device
Manuscript Type : Case Report
Page : 170-181
2
Page : 182-189Title : The Effect of Surface Treatments on Shear Bond Strength of Repaired Acrylic Denture Teeth with Resin Composite
Author(s) : Jirat Srihatajati, Pattarawadee Krassanairawiwong, Michell Veeraklaew, Thunyakamon Disakul, Piyawut Thitisakyothin, Thita Phinyoyang, Parima Rattanatikul
Keyword(s) : Surface treatment,Acrylic denture teeth,Resin composite,Shear bond strength,Bonding agent
Manuscript Type : Original Article (บทวิทยาการ)
Page : 182-189
3
Page : 190-197Title : Effect of Oral Simvastatin on Reduction of Periodontal Attachment loss: Observational study
Author(s) : Pichaya Wairojanakul, Pusadee Yotnuengnit
Keyword(s) : Oral Simvastatin,clinical attachment loss reduction,periodontal attachment loss reduction
Manuscript Type : Original Article (บทวิทยาการ)
Page : 190-197
Twenty-six patients were taking 5 or 10 mg/day, and 15 patients were taking 20 or 40 mg/day. They were in supportive periodontal treatment for 6 to 24 months. Medical history, medications and supplements, dosage and durations of simvastatin taken, and serum lipid levels were reviewed. Simplified Oral Hygiene Index was measured. Clinical attachment loss was recorded and compared site by site with the records at last maintenance visit. The percentage of sites which changes ≥ 2 mm either reduction or increment were calculated. Two independent sample t-tests, Spearman rank correlation, Pearson correlation, and multiple linear regression were used. P-value < 0.05 was considered significant. The average percentage of sites with clinical attachment loss reductions ≥ 2 mm in the group taking simvastatin doses 5 or 10 mg/day, and 20 or 40 mg/day were 11.18 ± 6.65 and 10.38 ± 6.91 respectively. These were not found to be significantly different nor was there evidence of a dose-response effect. Oral hygiene was found to be related with the reduction. The dose of oral simvastatin is not associated with a reduction of periodontal attachment loss.
4
Page : 198-208Title : Effect of Fluoride Varnish with Xylitol-coated Calcium and Phosphate Versus Fluoride Varnish on Early Childhood Caries Prevention at 6-Month Follow-up: A Randomized Control Trial
Author(s) : Onauma Angwaravong, Sujitra Soontornpakornkij, Waranuch Pitiphat, Thidarat Angwarawong
Keyword(s) : Calcium phosphate,Children,Dental caries,Fluoride varnish,Primary teeth
Manuscript Type : Original Article (บทวิทยาการ)
Page : 198-208
5
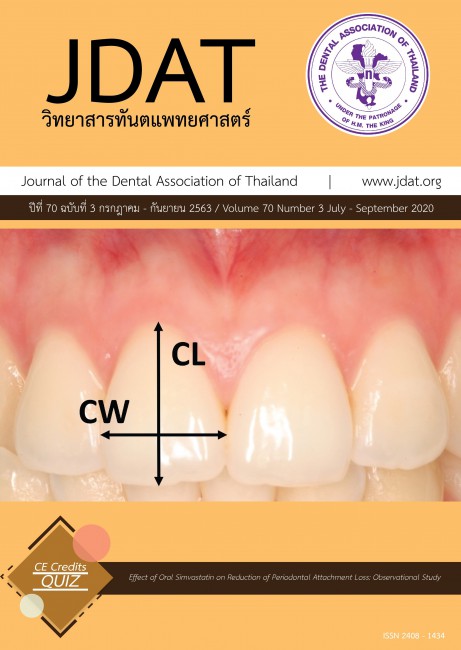
Page : 209-215Title : Analysis of Maxillary Incisor Tooth Dimensions and Gingival Phenotype in Thai Young Adults
Author(s) : Pimchanok Sutthiboonyapan, Kajorn Kungsadalpipob, Kanoktep Jamsakorn, Suphakrit Pumnil
Keyword(s) : Gingival phenotype,Gingival biotype,Maxillary incisors,Tooth dimension,Tooth proportion
Manuscript Type : Original Article (บทวิทยาการ)
Page : 209-215
6
Page : 216-229Title : Comparison of Retention between Two Implant Attachment Systems after Fatigue Test
Author(s) : Kittithorn Lertsuriyakarn, Mali Palanuwec
Keyword(s) : Fatigue test,Implant attachment,Implant overdenture retention,Retentive force
Manuscript Type : Original Article (บทวิทยาการ)
Page : 216-229
7
Page : 243-251Title : Effects of Orthodontic Treatment on the Upper Airway Dimension in Nongrowing Patients
Author(s) : Bancha Samruajbenjakun, Chonticha Kitiwiriyakul
Keyword(s) : Cephalogram,Orthodontics,Skeletal pattern,Upper airway
Manuscript Type : Original Article (บทวิทยาการ)
Page : 243-251
8
Page : 230-242Title : Cross-Sectional Microhardness of Area Adjacent to Cemented Bands
Author(s) : Somkamol Vanichvatana, Chawalid Pianmee, Thipawan Tharapiwattananon
Keyword(s) : Enamel demineralization,Orthodontic band cement,Cross-sectional microhardness
Manuscript Type : Original Article (บทวิทยาการ)
Page : 230-242
1
Page : 83-93Title : Titanium and Titanium Alloys in Implant Dentistry
Author(s) : Kavita Kanjanamekanant
Keyword(s) : Osseointegration,Titanium,Implants
Manuscript Type : Review Article (บทความปริทัศน์)
Page : 83-93
2
Page : 94-105Title : Masticatory Muscle Responses to Mandibular Forward Positioning Appliances
Author(s) : Napat Nalamliang, Udom Thongudomporn
Keyword(s) : Electromyography,Masticatory Muscles,Orthodontic Appliances,Functional
Manuscript Type : Review Article (บทความปริทัศน์)
Page : 94-105
3
Page : 106-116Title : Management of a Traumatized Maxillary Left Central Incisor by Moving the other Central Incisor across the Midline
Author(s) : Pornhathai Liewsaitong, Sikkared Parinyachaiphun, Thanit Charoenrat, Niranlarp Rerksanan
Keyword(s) : Midline crossing,Root resorption,Traumatized tooth
Manuscript Type : Case Report
Page : 106-116
4
Page : 117-123Title : Sectional Impression Trays with An Interlocking Handle Using Implant Impression Components to Fabricate Interim Dentures for A Patient with Scleroderma-induced Microstomia
Author(s) : Watcharapong Aroonsang, Surasak Yowcharoensuk
Keyword(s) : Microstomia,Scleroderma,Sectional tray
Manuscript Type : Case Report
Page : 117-123
5
Page : 124-138Title : Anti-biofilm Activity of Sericin Extract Coated on Titanium by Polyelectrolyte Multilayer Film Technique
Author(s) : Thidarat Angwarawong, Nopchanok Kaewwichian, Panisa Phukrongthaw, Onauma Angwaravong
Keyword(s) : Anti-biofilm activity,Sericin,Polyelectrolyte multilayers film,Titanium
Manuscript Type : Original Article (บทวิทยาการ)
Page : 124-138
6
Page : 139-149Title : Relationship between Symphysis Dimensions and Mandibular Incisors’ Alveolar Bone Thickness in Different Vertical Skeletal Patterns
Author(s) : Phuntin Uengkajornkul, Korapin Mahatumarat, Soontra Panmekiate
Keyword(s) : Alveolar bone thickness,Cone-beam computed tomography,Mandibular incisors,Mandibular symphysis,Vertical skeletal pattern.
Manuscript Type : Original Article (บทวิทยาการ)
Page : 139-149
7
Page : 150-157Title : The Effect of Various Types of Silane Coupling Agents on The Wettability of Hydrofluoric Acid-Etched/Unetched Lithium Disilicate Surfaces
Author(s) : Tool Sriamporn, Tanapon Tarateeraseth, Niyom Thamrongananskul
Keyword(s) : Contact angle,Hydrofluoric acid,Lithium disilicate,Silane coupling agent,Surface treatment
Manuscript Type : Original Article (บทวิทยาการ)
Page : 150-157
8
Page : 158-169Title : Influence of Type and Thickness of CAD-CAM Resin Ceramic on Micro-tensile Bond Strength to Dentin
Author(s) : Sirivimol Srisawasdi, Seelassaya Leelaponglit, Yanee Tantilertanant
Keyword(s) : CAD-CAM resin ceramic,Material thickness,Micro-tensile bond strength
Manuscript Type : Original Article (บทวิทยาการ)
Page : 158-169
1
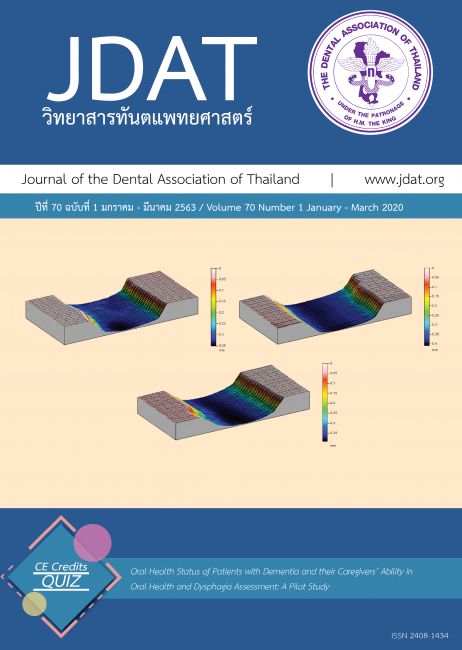
Page : 1-10Title : Oral Health Status of Patients with Dementia and their Caregivers’ Ability in Oral Health and Dysphagia Assessment: A Pilot Study
Author(s) : Orapin Komin, Panatcha Weerapol
Keyword(s) : Caregiver,Dementia,Dysphagia,OHAT,Oral health status
Manuscript Type : Original Article (บทวิทยาการ)
Page : 1-10
The aim of this study is to investigate the oral health status of dental patients with dementia and to evaluate the ability of caregivers of patients with dementia in primary oral health assessment using the Oral Health Assessment Tool (OHAT) and dysphagia detection using the Eating Assessment Tool (EAT-10). Nine dementia patients with their caregivers were voluntarily gave consented to participate in the study. Their oral health status and tongue pressure were recorded by oral examination and tongue pressure sensor device. Socio-demographic data, individual information, primary oral health assessment, OHAT, EAT-10, and any symptom-sign correlation of dysphagia was derived from an interview with caregivers. Descriptive statistics were reported by the mean with SD and percentage. The mean age of participants was 83.33 (±4.15) years old. The average remaining teeth was 11.22 (±9.74). Seven participants (77.8 %) had fixed and/or removable dental substitution. Only 33.3 % had at least 20 functional teeth, while 22.2 % had at least four Posterior Occluding Pairs. Almost half of the participants (44.4 %) had periodontal disease, and two (22.2 %) had active dental caries. For the tongue pressure value, four (44.4 %) had a substandard tongue pressure value (less than 20 kPa) which implied the risk of dysphagia. While three out of these four cases can be detected for dysphagia signs by their caregivers using EAT-10. For the OHAT assessment, 55.6 % of the caregivers had similar OHAT scores with dental professionals. The differences between caregivers and dental professionals in their OHAT assessment were in the sections of oral cleanliness, the status of natural teeth, and the quantity of saliva, while the largest frequency of agreements were lips, dentures, and dental pain. The results showed that the oral health of the patients with dementia is not so good as almost half of the participants have a problem with periodontal disease and 70% have less than 20 natural teeth. Also almost 80 % have less than four occluding pairs. However, caregivers have the potential in dysphagia early detection and the ability in oral health assessment which indicate the need for further study and to develop a training program for caregivers.
2
Page : 11-25Title : Effects of Palaseal® Coating Agent on Surface Roughness of Heat-polymerized Denture Base Acrylic Resins
Author(s) : Duangjai Uraivichaikul, Issarawan Boonsiri, Kamolporn Wattanasirmkit
Keyword(s) : acrylic resins,coating agents,Palaseal®,surface coating,surface roughness
Manuscript Type : Original Article (บทวิทยาการ)
Page : 11-25
The objective of this study was to evaluate effects of Palaseal® on surface roughness of acrylic resins which passed different polishing techniques. One hundred eighty heat-polymerized polymethymethacrylate specimens
were fabricated and finished with abrasive sandpaper. Then they were randomly equally divided into six groups. A control group (N) was neither polished nor Palaseal® coated. The others were experimental groups as follows: No polishing with Palaseal® coating (NC), pumice and Tripoli polishing without coating (P), pumice and Tripoli polishing with coating (PC), silicone points polishing without coating (S), silicone points polishing with coating (SC). Changes in surface roughness were measured with a profilometer and calculated Ra of specimens. SEM was utilized for surface visualization and surface roughness confirmation. Two-way ANOVA and Tukey Honestly Significant Difference (HSD) were used for statistical analysis. Group (N) had the highest mean Ra value (670.5 nm.) whereas group (PC) had the lowest mean Ra value (241.9 nm.). Groups (N, NC) had the mean Ra value (670.5, 394.5 nm.) significantly (P<0.01) more than groups (S, SC) (300.1, 254.9 nm.) and groups (P, PC) (283.2, 241.9 nm.) respectively. Differences of the mean Ra values between Palaseal® uncoated groups (N, P, S) and coated groups (NC, PC, SC) were statistically significant (P<0.01). Lastly, there was interaction between surface polishing and Palaseal® coating. Palaseal® coating on heat polymerized acrylic resins enhanced surface smoothness of acrylic resins polished with pumice and Tripoli and silicone points, including finished with abrasive sandpaper.
3
Page : 26-35Title : Factors Affecting the Failure of Class II SMART Restorations in Mandibular Primary Molar Teeth in Preschoolers Participating in the Dental Proactive Project of Public Health Region 12
Author(s) : Pichanun Srisommai, Suda Saetiew, Oitip Chankanka, Duangthida Paiboonwarachart
Keyword(s) : Glass ionomer cement,Primary teeth,Dental caries,Restorative technique,ART
Manuscript Type : Original Article (บทวิทยาการ)
Page : 26-35
Objectives: This study aimed to assess associations between occluso-proximal caries related factors and success/failure of class II restorations in mandibular primary molar teeth using the SMART technique and to assess failure characteristics of Class II restorations using the SMART technique in mandibular primary molar teeth. Methods: This study was approved by the Ethics Committee at The Faculty of Dentistry, Prince of Songkla University.
Children aged 3-5 years old having dentinal caries on occluso-proximal surfaces were recruited for this study. One hundred and forty-one teeth were examined for clinical information regarding caries lesions and related factors. Dental models were cast from putty silicone impressions. For all selected teeth, soft caries was removed by spoon excavators and then restored with glass ionomer cement (Fuji IX GP Extra capsule, GC Corp., Japan) by dental therapists as part of an ongoing regular project. Clinical examination for ART scores was conducted at 6-month follow-up. Multivariable logistic regression analyses were conducted. Results: The success rate of SMART Class II restorations was 70.7 %. Based on the multivariable logistic regression model, occluso-distal lesion in the primary mandibular first molar, interproximal gingival inflammation and interproximal space were statistically significantly associated with higher failure rate of SMART Class II restorations. Loss of restoration was the most common failure for the restorations. Conclusions: For SMART Class II restorations having an occluso-distal lesion in primary first molars, having adjacent interproximal gingival inflammation and having interproximal space were more likely to fail in SMART Class II restorations.
4
Page : 36-44Title : Consistency of Orthodontic Treatment Need Indexes in the Community between Orthodontist, General Dentist and Dental Nurse
Author(s) : Angkana Thearmontree, Rongrong Promchan, Supanee Suntornlohanakul
Keyword(s) : Orthodontic treatment need,Community Orthodontic Treatment Need index,Dental Aesthetic Index,Dental nurse,General dentist
Manuscript Type : Original Article (บทวิทยาการ)
Page : 36-44
The objective of this study was to evaluate the consistency and time consumed of the Community Orthodontic Treatment Need (COTN) index that was developed by researchers from the Faculty of Dentistry, Prince of Songkla
University compared with the Dental Aesthetic Index (DAI). The samples consisted of 80 students (18 males and 62 females) aged 15 to 20 years (17.6±1.6 years) in Hat Yai, Songkhla. The samples were examined with DAI
and COTN indexes by orthodontist, standardized and well-trained general dentist and dental nurse. Statistical analysis included the Kappa coefficient and paired t-test. Result: Both indexes had good consistency between examiners but COTN was more consistent than DAI. The inter-examiner consistency between orthodontist and general dentist was higher than for orthodontist and dental nurse (Kappa of DAI=0.709 and 0.618, Kappa of COTN=0.717 and 0.623, respectively). When comparing the times consumed between DAI and COTN indexes, the results revealed no significant difference in time consumption between the orthodontist and general dentist (P>0.05) but dental nurse used significantly more time to examine both indexes than orthodontist (P<0.01). In addition, dental nurse used significantly less time with COTN than DAI (P=0.001). This study concluded that well-trained dental nurse and general dentist were able to determine orthodontic treatment need using both indexes. Higher consistency and less time consumption were found when performing with the COTN index compared to the DAI index.
5
Page : 45-53Title : Evaluation of the Push-out Bond Strength of MTA-based Sealer in the Simulated Immature Root Models
Author(s) : Sirikul Wanapaisarn, Nateetorn Plukwatchalakul, Peeraporn Taweewattanapaisan, Chinalai Piyachon
Keyword(s) : Push-out bond strength,Root canal sealer,MTA
Manuscript Type : Original Article (บทวิทยาการ)
Page : 45-53
The aim of this study was to compare the push-out bond strength of MTA Fillapex to AH Plus and CU Sealer in simulated immature root models. The models were created from forty-five extracted single root premolars and
randomly divided into three groups of fifteen each. Root canals were obturated with gutta-percha and one of thefollowing sealers: MTA Fillapex, AH Plus and CU Sealer. After immersion in phosphate buffered saline for twenty-eight days, the roots were cut perpendicularly to the long axis to create 3-mm thick slices from the apical end of roots. The push-out bond strength was measured with a universal testing machine. Failure modes were determined under scanning electron microscopy. The highest mean of push-out bond strength was found in AH Plus group, followed by MTA Fillapex and CU Sealer sequentially at p<0.05. Within the limitations of this in vitro study, MTA Fillapex showed less push-out bond strength to root dentin when compared to AH Plus sealer.
6
Page : 54-62Title : The Comparison of the Effect of Antacid and Remineralizing Agent on the Prevention of Enamel Surface Loss and Microhardness of Human Enamel Exposed to Hydrochloric Acid
Author(s) : Krittaporn Jomthepmala, Vasana Patanapiradej
Keyword(s) : Hydrochloric acid,Enamel surface loss,Microhardness,Antacid,Remineralizing agent
Manuscript Type : Original Article (บทวิทยาการ)
Page : 54-62
The aims of this study were to compare the effects of antacid and remineralizing agent on the prevention of enamel surface loss and microhardness of enamel exposed to hydrochloric acid. Flat specimens on buccal enamel
surface of 60 extracted human premolar teeth were prepared. Each specimen was subjected to microhardness measurement to obtain a baseline value. The specimens were allocated into 3 groups (n=20) consisting of the
treatments: antacid, remineralizing agent and control group. All specimens were exposed to hydrochloric acid for 2 minutes. Then the specimens were either immersed in antacid for 2 minutes or applied remineralizing agent for 3 minutes depending on the experimental groups. Finally, the specimens were immersed in artificial saliva for 24 hours. The process was repeated for 5 cycles. The final microhardness and enamel surface loss were assessed. The data were analyzed statistically with the level of significance at p<0.05. Using Paired T-test to compare baseline and final microhardness within group, Welch ANOVA and Game-Howell multiple comparisons to compare baseline and final microhardness between groups, One-way ANOVA and Post hoc Turkey’s test to compare enamel surface loss between groups. The final microhardness of all groups was significantly lower than the baseline microhardness (p<0.001). Compared to control group, the final microhardness was significantly higher when using antacid and remineralizing agent (p=0.001 and 0.003 respectively) and the enamel surface loss was significantly lower when using antacid and remineralizing agent (p<0.001 and 0.006 respectively). The final microhardness and enamel surface loss between the antacid and remineralizing agent groups were not significantly different. From the result of this study, the effects of antacid and remineralizing agent on the prevention of enamel surface loss and microhardness of human enamel exposed to hydrochloric acid were not significantly different.
7
Page : 63-71Title : Comparison of Demineralization Resistance on Root Dentin of Calcium Silicate Based-material and Glass Ionomer Cement
Author(s) : Kitinee Wattanasookchai, Rangsima Sakoolnamarka
Keyword(s) : Glass ionomer cement,Demineralization resistance,Knoop microhardness,Root dentin,Calcium silicate based-material
Manuscript Type : Original Article (บทวิทยาการ)
Page : 63-71
The objective of this study was to compare the effect of calcium silicate based-material and glass ionomer cement on root dentin demineralization resistance. Sixty root dentin specimens from human permanent premolars were prepared to obtain standardized cavities and randomly divided into 4 groups (n=15): group1-negative control (no restoration), group 2- conventional glass ionomer cement, group 3-resin modified glass ionomer cement and group 4- calcium silicate based-materials. The surface knoop microhardness test was performed on root dentin at 50, 100, 150 and 200 μm from restoration margin. The specimens were subjects to pH-cycling model then, surface knoop microhardness test was measured again. Two specimens from each group were randomly selected to assess mineral composition in dentin adjacent to restorative materials using energy dispersive X-ray pectroscopy. Data were analyzed using two-way repeated measures ANOVA, one-way ANOVA and Tukey HSD test, repeated measures ANOVA and Bonferroni post-hoc test with the level of significance at p<0.05. Surface microhardness loss of root dentin from group 4 was significantly lower than the other groups in every distance from restoration margin. Surface microhardness loss of root dentin from group 2 and 3 was not significantly different but the surface microhardness loss from both groups was significantly different from group 1. From the results of this study, root dentin restored with calcium silicate based-material had higher demineralization resistance than root dentin restored with glass ionomer cement until 200 μm from restoration margin.
8
Page : 72-82Title : The Effects of 4 mg Dexamethasone on Anti-inflammation and Quality of Life after Surgical Removal of The Lower Third Molar: A Split-mouth Triple-blind Randomized Placebo-controlled Study
Author(s) : Laddawun Sununliganon, Thachaya Satavuthi, Chatchai Pesee, Takerngsuk Phetchuay, Phensiri Sangroongrangsri, Bhakajira Suppateepmongkol, Rinruedee Phothinamthong, Chatchai Sirirungseero
Keyword(s) : Anti-inflammation,Dexamethasone,Surgical removal of the third molar
Manuscript Type : Original Article (บทวิทยาการ)
Page : 72-82
Inflammatory complications following third molar surgery are a concern of patients. Dexamethasone, one of the corticosteroids, possesses an anti-inflammatory property that can reduce inflammation. However, there is no consensus on an appropriate administration. This study evaluated the anti-inflammatory outcomes of 4 mg dexamethasone given by pre-operative submucosal injection after the surgical removal of third molars. A split-mouth, randomized, triple-blind, placebo-controlled study was carried out with 17 participants (34 impacted teeth) having bilateral identical lower third molar impaction. Submucosal injection of either 4 mg dexamethasone or placebo was given after anesthetization of the inferior alveolar nerve according to random assignment. The time interval between the first and second operation was a 4week period. Single surgeon, assessor, and data analyst were arranged and they did not know of drug use. Onset and duration of local anesthetic were collected. On postoperative days 1, 2, 3 and 7, pain intensity was recorded using a visual analog scale. At baseline and postoperative days 1, 3 and 7, swelling and maximal mouth opening were measured. No effect of dexamethasone on swelling and mouth opening was detected when compared to control. However, dexamethasone injection group showed significantly less pain than control at every time points, p<0.05. The quality of life in the physical domain was better in dexamethasone injection group than control. For third molar surgery, 4 mg dexamethasone did not demonstrate a benefit in anti-swelling or improve mouth opening. However, it significantly reduced pain and improved quality of life.